The availability of high quality modular buildings has been a huge advantage for hospitals and health trusts faced with urgent need for additional facilities, and increased pressure on funding.
Rapidly deployed modular buildings can offer a design life of up to 60 years but can be delivered in a fraction of the time taken for conventional build methods, making them an attractive option.
However, there is a concern that the drive to get the best value is often driven simply by the lowest price or fastest turnround, without taking into account vital requirements for patient care, in particular infection control and patient comfort
One area of primary concern is ensuring appropriate ventilation of modular buildings that is compliant with the highest standards and not simply meeting the minimum requirements within guidance documents.
Many buildings are supplied with no mechanical ventilation or air-handling system. That may be considered adequate ventilation to meet those minimum standards, but adequate and appropriate are not the same thing.
Specific clean-air handling design for the internal configuration of each building should be a requirement to ensure appropriate air flow accommodating patients.
Ventilation is a crucial tool to protect patients and staff from the spread of potentially-harmful pathogens, and ensure their comfort and safety.
Infection prevention and control is vital in healthcare settings at any time, but that has been a primary focus during the recent COVID-19 pandemic.
Research into Coronavirus has indicated that the greatest danger of transmission is via aerosol-based routes and droplets carried in exhaled breath. Ventilation and airflow is therefore increasingly important.
When specifying a modular building and choosing a supplier, hospitals and health trusts need to carefully evaluate the need for clean-air ventilation and its impact on a specific space configuration. The underlying concept of factory-built accommodation is rapid production for a mass market at the cheapest price – not specifically designed and engineered modular building solutions for the medical sector.
Professor Cath Noakes from the School of Civil Engineering at the University of Leeds addressed the virtual Healthcare Estates Conference in October 2020 on the issue of ventilation.
Professor Noakes is leading research into ventilation, indoor air quality and infection control in the built environment.
She acknowledged that there is little data from real-world medical settings about COVID-19 transmission, but evidence from community settings shows the highest risk is probably within indoor environments and over short ranges.
In addition to droplets settling on surfaces, and the virus transmitting directly between people during physical contact; there is also evidence of airborne transmission of COVID-19, particularly in poorly-ventilated spaces.
People are at their most contagious when they are largely asymptomatic, so that it becomes increasingly important to consider ventilation of spaces housing patients.
She pointed out that airborne aerosol particles need drag force to keep them up and gravity to bring them down. But air velocity in a room is known to impact on this and various-sized particles can remain in the air for a significant amount of time, often travelling quite far from their original source.
This is where clean-air ventilation can have a significant impact.
“If a space is well ventilated you can’t completely contain the virus, but the ventilation will dilute the virus and the risks are technically lower,” reasoned Professor Noakes.
This view is reflected in the Federation of European Heating, Ventilation and Air Conditioning Association’s recently-updated REHVA COVID-19 Guidance Document, which cites ventilation as the principal engineering control to help control infection, thus giving further weight to the vital role ventilation plays in the COVID-19 response effort.
It states that in hospitals with an optimal 12 air changes per hour (ACH) ventilation rate, aerosol transmission is mostly eliminated. But, in poorly-ventilated spaces, it may be dominant.
Professor Noakes suggests that in a hospital context it is not the obvious patient wards that will be most affected as these tend to be better ventilated.
Instead, estates and facilities managers and IPC teams need to also consider smaller, more-relaxed environments such as staff restrooms, waiting areas, corridors and treatment rooms.
“Hospitals need to consider where they are ventilating and what impact this has on a particular space,” Professor Noakes said.
However, mechanical ventilation is not provided in the standard specification of modular buildings. Compliance with HTM 03-01 simply means that the supplier has met the minimum standards required. In addition, as with any natural ventilation method, the air flow and air change rates cannot be guaranteed as they are subject to external factors such as wind speed and direction.
The HTM 03-01 standard dates back to 2007, and therefore does not take into account the latest thinking on the need for clean-air design within the types of modular buildings increasingly used by hospitals for patient accommodation.
When it was produced in 2007 the use of modular buildings was very limited, but now they are seen as vital tool for increasing healthcare facilities. An updated version of HTM 03-01 due for publication early in 2021 has received specialist input to address the latest thinking on clean-air requirements in patient accommodation.
Ventilation systems are complex solutions and their impact depends on the type of technology and, critically, how it is deployed.
The risks faced by healthcare workers treating patients with viruses that can be transmitted through the air are highlighted by research published in August 2020 by the Institution of Occupational Safety and Health (IOSH).
Researchers from University Hospitals of Leicester NHS Trust in the UK and Turku University of Applied Sciences in Finland examined these risks and how different forms of ventilation can protect staff who are treating patients in hospital isolation rooms, the study, called ‘Reducing aerosol infection risk in hospital patient care’, was commissioned by IOSH because while the risks to frontline healthcare workers when caring for patients with viruses are well known – less known is the optimal design of mechanical ventilation systems. The aim was to see how an engineering control approach of optimising ventilation methods can reduce these risks.
Dr Julian Tang, a consultant virologist at the University Hospitals of Leicester NHS Trust and an honorary associate professor at the University of Leicester, argues that: “The most-effective form of control is the ventilation engineering level of control.
“That means that we have to try and improve the amount of clean-air in the environment compared to the amount of contaminated air.
“The research has shown that there are certain types of ventilation – beyond just different speed and volume of ventilation – that can benefit healthcare workers better without being detrimental to the patient.
“And this report has tried to highlight those particular designs to show that if you are going to build a new hospital with new isolation rooms, these sorts of design are what you might want to follow.”
David Hartley, managing director at medical modular building specialist MTX welcomes the report: “The IOSH report focuses particularly on treating patients in isolation rooms, which are typically provided with a minimum of 10 air changes per hour of mechanical ventilation. It underlines the importance of mechanical ventilation in reducing airborne aerosol infection.
“At MTX we recognise the importance of engineering air movement and clean-air flow pathways within modular buildings – particularly those housing patients. Those factors are a vital consideration for our engineers when assessing the performance of the buildings we provide for health trusts and hospitals. We have the technical expertise and experience to work with clinicians and facilities teams to ensure the building is fit for purpose in every case.
“Optimum airflow is accepted as an important factor in the health, wellbeing and comfort of patients and staff. It is much more difficult and expensive to retrofit air handling systems to modular units, which is why it is so important to give it full consideration at the design and build stages.”

David Guilfoyle, a director at consulting M&E engineers DSSR which works with MTX adds: “Ventilation has become much more of an issue with the emergence of COVID-19, and it has reshaped the priorities for ventilation requirements. We work with MTX to ensure that the air handling provision is effective, bringing maximum benefit and enhancing the safety of patients and staff.”
DSSR designs central air handling for each modular unit produced by MTX according to how it will be used, the patient group and the internal configuration.
Mr Guilfoyle explains: “You have to walk in the shoes of the people who will be working in that building. If you simply follow the basic HTM guidance you are not walking in their shoes. HTM is a baseline, not a target “Without talking to the clinicians and the infection control team you cannot possibly design an air handling system that is fit for purpose. You must know the configuration of the beds and know how they are to be used. Then you can design the system around the clinical requirements, not simply pump air into the room. The configuration, positions of walls and corridors all influence the effectiveness of the air handling system.
“For example, people talk about 6 or 12 air changes per hour (ACH) ventilation rate in terms of volume, but that rate depends on the configuration. Previously one of the priorities for air exchange was mitigating the effects of medical gases that could affect staff. Now it is more about infection control – a priority that has gained momentum over the last year.
“Six ACH may be quite appropriate for one layout, but a different layout occupying the same floor space may require 12. It is a bespoke solution every time with MTX, and clients get the benefit of flexible M&E design by experts in their field who understand the needs of staff and patients.
“We must also take into account air dilution rates – which reduce the particulate content of the air – a vital tool in reducing airborne infection of a virus like COVID-19. In addition, clean-air pathways can be custom-designed according to the configuration of each individual modular building.
“If you want to capture the ‘bad air’ and vent it – then it all comes down to the pathways you create through the design of the system.”
Mr Hartley points out that factory-built units are too often simply mass-produced shells; they are not engineered for a specific purpose which may vary from one hospital site to the next.
“It is not one-size fits all. For example, people who deliver a building in just a few short weeks may be working hard to fulfil a need – but the building they produce may be a basic shell which could as easily be a schoolroom or an office. Modular buildings used for patient care should be specifically designed and engineered for healthcare use.”
“Taking into account the threat from COVID-19 it is apparent that more attention needs to be paid to ensuring mechanical ventilation is considered in every case when designing and creating modular buildings.”
DSSR has been involved as a technical expert in updating the HTM 03-01 memorandum to make it more fit for purpose in modern healthcare. The new version is currently being ratified for publication early in 2021.
www.mtxcontracts.co.uk




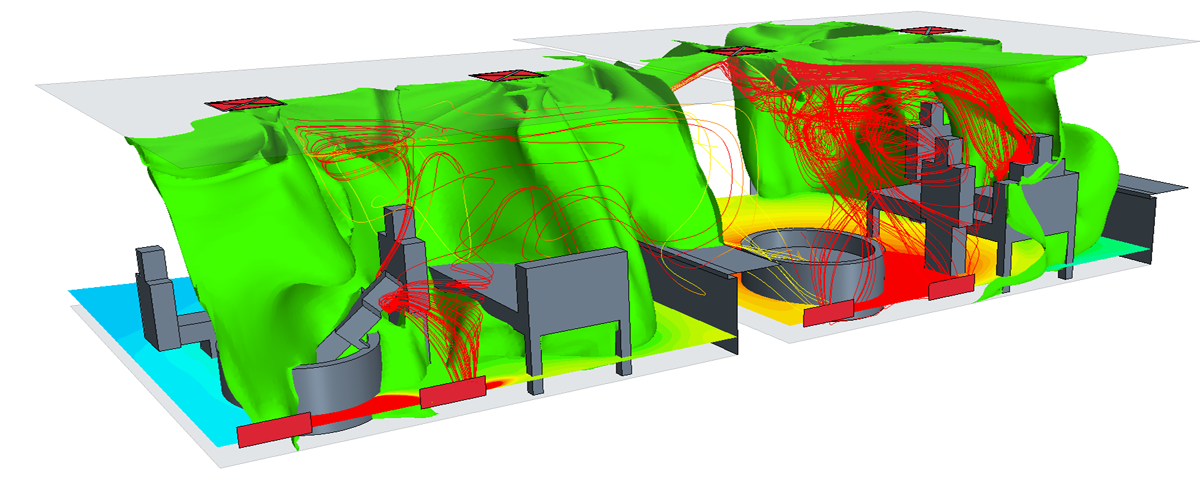




 Fig 1 (produced by STA) shows how a CLT structure is built up with the correct installation of insulation, on the outside of the frame. The CLT should always be on the warm side of the insulation to avoid unnecessary moisture fluctuations, which also brings the added benefit of mitigating any potential cold bridging issues, as they are adequately catered for with the external envelope of continuous insulation. It is preferable for this insulation to be moisture open to allow the wall to breathe and reduce the risk of built-up moisture within the envelope. The cavity provides extra protection throughout the life of the building. The STA have produced further guidance in January this year (Laminate/Mass timber structures – Durability by Design Technical Note 23). This note concludes with some best practice advice which includes the following – Ensure the external wall make up allows for vapour diffusion from the interior to exterior vented spaces (BS5250 standard to be referenced and followed in a design). Air leakage control membranes and sealants checked to avoid moisture vapour traps. Thermal Insulation should be placed on the exterior side of the laminated mass timber panels.
Fig 1 (produced by STA) shows how a CLT structure is built up with the correct installation of insulation, on the outside of the frame. The CLT should always be on the warm side of the insulation to avoid unnecessary moisture fluctuations, which also brings the added benefit of mitigating any potential cold bridging issues, as they are adequately catered for with the external envelope of continuous insulation. It is preferable for this insulation to be moisture open to allow the wall to breathe and reduce the risk of built-up moisture within the envelope. The cavity provides extra protection throughout the life of the building. The STA have produced further guidance in January this year (Laminate/Mass timber structures – Durability by Design Technical Note 23). This note concludes with some best practice advice which includes the following – Ensure the external wall make up allows for vapour diffusion from the interior to exterior vented spaces (BS5250 standard to be referenced and followed in a design). Air leakage control membranes and sealants checked to avoid moisture vapour traps. Thermal Insulation should be placed on the exterior side of the laminated mass timber panels.




